Your gut is having a conversation with your brain right now. And if you’ve been feeling anxious, foggy, or just “off” lately, you might be surprised to learn that the problem—and the solution—could be sitting in your digestive system.
Welcome to the era of the gut-brain axis, where scientists are discovering that the key to better mental health might not be found in your medicine cabinet, but in your kitchen. According to the National Institute of Mental Health, over 50 million Americans experience mental illness annually, and emerging research suggests gut health plays a more significant role than previously understood.
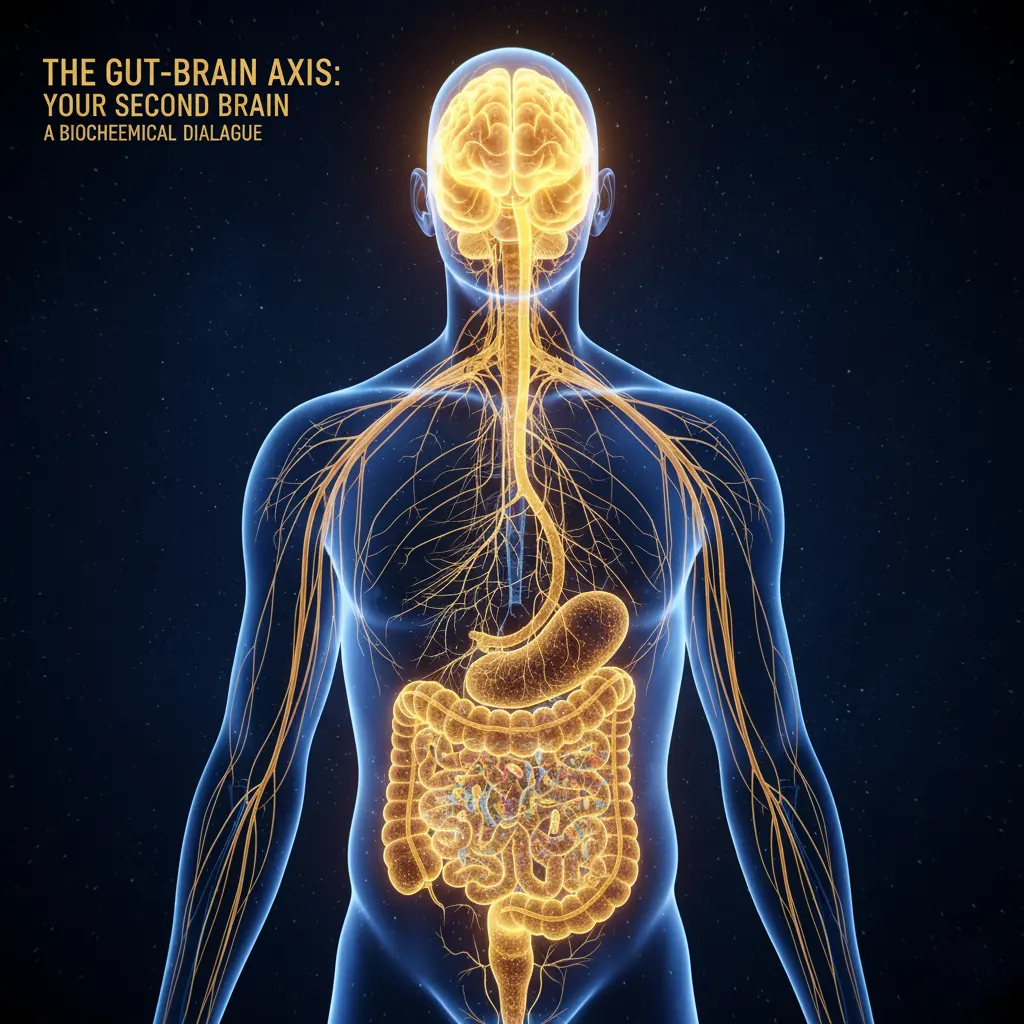
Understanding the Gut-Brain Connection: Your Second Brain
Inside your gut lives a bustling metropolis of roughly 100 trillion microorganisms—bacteria, fungi, and other microbes collectively known as your gut microbiome. This isn’t just a passive ecosystem; it’s a biochemical powerhouse that produces up to 90% of your body’s serotonin, the neurotransmitter most associated with happiness and well-being.
Think about that for a moment. The same “feel-good” chemical that antidepressants aim to boost is being manufactured right now in your intestines. Your gut also produces significant amounts of dopamine, GABA, and other neurotransmitters that regulate mood, motivation, and anxiety levels.
The gut-brain connection works through multiple pathways. Research published by Harvard Medical School explains that the gut and brain communicate constantly through the vagus nerve, immune system signals, and the metabolites produced by your gut bacteria. These interactions influence everything from stress response to cognitive function and emotional regulation.
The Science Behind Gut Health and Mental Health
The research linking gut health to mental wellness is compelling. Studies have found that people with depression and anxiety often have distinctly different gut microbiomes compared to those without these conditions. It’s a bidirectional relationship: chronic stress can damage your gut lining and alter your microbiome composition, while an unhealthy gut can trigger systemic inflammation that affects brain function and mood regulation.
According to the American Psychological Association, the gut-brain axis is now recognized as a critical factor in mental health treatment. This connection explains why so many people with irritable bowel syndrome (IBS) also experience anxiety and depression, and vice versa.
Americans face particular challenges. Our standard American diet (SAD)—high in processed foods, refined sugars, and artificial additives—creates a hostile environment for beneficial gut bacteria while feeding pathogenic strains. Combine this with antibiotic overuse, chronic stress, inadequate sleep, and sedentary lifestyles, and you have a perfect storm for both digestive and mental health problems.
The symptoms manifest in ways you might not expect: brain fog, irritability, difficulty concentrating, mood swings, heightened anxiety, or that persistent low-level depression that colors your entire day. You might blame work stress or burnout, but your gut microbiome could be the underlying culprit.
15+ Best Foods for Gut Health and Mental Wellness
The good news? You can start rebuilding a healthier gut-brain connection today with strategic food choices. Here are the most effective foods backed by scientific research:
Fermented Foods: Natural Probiotics for Anxiety and Depression
Fermented foods are like sending reinforcements to your gut’s beneficial bacteria. The live cultures in these foods directly populate your gut and produce mood-boosting compounds like GABA and short-chain fatty acids.
Top fermented foods for mental health:
- Greek yogurt and kefir: Rich in Lactobacillus and Bifidobacterium strains linked to reduced anxiety
- Sauerkraut and kimchi: Contain multiple probiotic strains and vitamin C for stress resilience
- Kombucha: Provides probiotics, B vitamins, and organic acids that support gut lining
- Miso and tempeh: Fermented soy foods rich in probiotics and protein
- Pickles (naturally fermented): Look for refrigerated varieties with live cultures
Start with small amounts if you’re new to fermented foods—even 2-3 tablespoons of sauerkraut or a 4-ounce glass of kefir daily can make a noticeable difference within weeks.
Prebiotic Fiber Foods: Feeding Your Good Gut Bacteria
While probiotics add beneficial bacteria, prebiotics feed the ones already colonizing your gut. These special types of fiber are fermented by gut bacteria into short-chain fatty acids like butyrate, which reduce inflammation and support brain health.
Best prebiotic foods:
- Garlic and onions (raw or cooked)
- Leeks and asparagus
- Jerusalem artichokes
- Bananas (especially slightly green)
- Oats and barley
- Apples and berries
- Chicory root and dandelion greens
- Flaxseeds and chia seeds
The Academy of Nutrition and Dietetics recommends 25-38 grams of total fiber daily, with a significant portion coming from prebiotic sources for optimal gut and mental health.
Omega-3 Fatty Acids: Essential Fats for Brain and Gut Health
Omega-3 fatty acids reduce gut inflammation while supporting neurotransmitter function and brain cell membrane integrity. The EPA and DHA forms found in fatty fish are particularly beneficial for mental health.
Top omega-3 sources:
- Wild-caught salmon, sardines, mackerel, and anchovies (2-3 servings weekly)
- Walnuts (handful daily)
- Chia seeds and ground flaxseeds (1-2 tablespoons daily)
- Hemp seeds
- Algae-based supplements (for vegans)
Research shows omega-3s can be as effective as some medications for mild to moderate depression, particularly when combined with improved gut health.

Polyphenol-Rich Foods: Antioxidants That Feed Good Bacteria
Polyphenols are plant compounds that act as both antioxidants and prebiotics. Your gut bacteria metabolize them into beneficial compounds that reduce inflammation and support cognitive function.
Best polyphenol sources:
- Berries (blueberries, strawberries, blackberries)
- Dark chocolate (70% cacao or higher)
- Green tea and matcha
- Extra virgin olive oil
- Coffee (in moderation)
- Red cabbage and purple sweet potatoes
- Nuts, especially pecans and hazelnuts
Tryptophan-Rich Protein Foods: Building Blocks for Serotonin
Your body needs the amino acid tryptophan to produce serotonin. While most serotonin is made in the gut, ensuring adequate tryptophan intake supports both gut and brain production.
Top tryptophan sources:
- Turkey and chicken
- Eggs (especially pasture-raised)
- Wild-caught fish
- Grass-fed beef
- Pumpkin seeds and sesame seeds
- Chickpeas and lentils
- Organic tofu and tempeh
For optimal serotonin production, pair tryptophan-rich foods with complex carbohydrates like sweet potatoes, quinoa, or brown rice.
Glutamine and Bone Broth: Healing the Gut Lining
L-glutamine is an amino acid that helps repair and maintain the intestinal barrier, preventing “leaky gut” that can trigger systemic inflammation and mood disorders.
Best sources:
- Bone broth (homemade or high-quality store-bought)
- Grass-fed beef and chicken
- Wild-caught fish
- Eggs
- Cabbage and asparagus
- L-glutamine supplements (consult a healthcare provider)
Anti-Inflammatory Whole Foods
Chronic inflammation disrupts both gut health and mental wellness. These foods actively combat inflammation:
- Turmeric and ginger
- Leafy greens (spinach, kale, Swiss chard)
- Beets
- Fatty fish
- Green tea
- Colorful vegetables (bell peppers, tomatoes, carrots)
Foods to Avoid: Gut Disruptors That Harm Mental Health
Just as important as what you add is what you minimize. According to the Cleveland Clinic, these foods can damage gut health and worsen mental health symptoms:
Limit or avoid:
- Refined sugars and high-fructose corn syrup: Feed harmful bacteria and cause blood sugar crashes
- Artificial sweeteners: Disrupt gut bacteria balance and may worsen anxiety
- Processed foods with emulsifiers: Damage gut lining (carrageenan, polysorbate 80, CMC)
- Excessive alcohol: Disrupts microbiome and increases gut permeability
- Trans fats and hydrogenated oils: Promote inflammation
- Heavily processed meats: Contain additives that harm gut bacteria
- Gluten (for sensitive individuals): Can trigger inflammation and mood changes
You don’t need perfection, but reducing these items by 80% can yield noticeable improvements in both digestion and mood within 2-4 weeks.

Best Probiotics for Mental Health and Anxiety
While whole foods should be your foundation, high-quality probiotic supplements can accelerate gut healing and mood improvement. Look for products containing these research-backed strains:
Most effective probiotic strains for mental health:
- Lactobacillus rhamnosus: Reduces anxiety and stress hormones
- Bifidobacterium longum: Improves stress response and reduces cortisol
- Lactobacillus helveticus: Combined with B. longum, reduces anxiety and depression
- Bifidobacterium breve: Supports mood regulation
- Lactobacillus plantarum: Reduces inflammation and supports cognition
Choose probiotics with:
- At least 10-50 billion CFUs per serving
- Multiple strains (diversity matters)
- Third-party testing for quality
- Delayed-release or enteric-coated capsules
- Refrigeration (for most products)
Consult with a healthcare provider before starting supplements, especially if you have compromised immunity or take medications.

Daily Gut Health Routine for Better Mental Health
Eating well is crucial, but lifestyle practices amplify the benefits. Here’s a comprehensive daily routine:
Morning Routine (6-9 AM)
Hydration First: Start with 16 ounces of room-temperature water with fresh lemon juice to stimulate digestion and support liver detoxification.
Probiotic-Rich Breakfast: Within an hour of waking, eat a gut-healthy breakfast:
- Greek yogurt parfait with berries, chia seeds, and walnuts
- Eggs with sauerkraut and avocado on whole grain toast
- Overnight oats with kefir, flaxseeds, and blueberries
Morning Movement: 10-20 minutes of gentle movement (walking, yoga, stretching) stimulates gut motility and reduces stress hormones.
Midday Routine (12-3 PM)
Balanced Lunch: Include protein, fiber, and fermented foods:
- Grain bowl with salmon, kimchi, leafy greens, and tahini
- Chicken salad with mixed vegetables and olive oil dressing, served with pickles
- Lentil soup with bone broth base and cultured vegetables
Prebiotic Snacks: When hunger strikes between meals:
- Apple slices with almond butter
- Hummus with raw vegetables (carrots, bell peppers, jicama)
- Handful of walnuts with dark chocolate
- Banana with a tablespoon of chia seeds
Stress Management Break: Take 5-10 minutes for deep breathing, a brief walk, or meditation. This activates your vagus nerve and improves gut-brain communication.
Evening Routine (6-10 PM)
Early, Mindful Dinner: Eat at least 3 hours before bed to allow proper digestion:
- Wild-caught fish with roasted vegetables and quinoa
- Grass-fed beef with sweet potato and fermented vegetables
- Tofu stir-fry with cruciferous vegetables over brown rice
Post-Dinner Walk: A gentle 15-20 minute walk aids digestion and blood sugar regulation.
Gut-Healing Evening Ritual:
- Herbal tea (chamomile, ginger, or peppermint) 1-2 hours before bed
- Probiotic supplement if using
- Light stretching or restorative yoga
- Digital sunset (screens off 1 hour before sleep)
Sleep Optimization: Aim for 7-9 hours in a cool (65-68°F), dark room with consistent sleep and wake times. Your microbiome has its own circadian rhythm, and disrupting it damages gut health and mood.
Weekly Practices
- Meal prep: Dedicate 2-3 hours weekly to prepare fermented foods, bone broth, and healthy meals
- Fasting window: Consider a 12-14 hour overnight fast (e.g., 7 PM to 9 AM) to support gut repair
- Nature time: Spend at least 2 hours weekly outdoors for stress reduction and vitamin D
- Social connection: The Centers for Disease Control and Prevention emphasizes that social wellness impacts both mental health and gut function
Exercise and Movement for Gut-Brain Health
Regular physical activity diversifies your gut microbiome, reduces inflammation, and boosts mood-regulating neurotransmitters. You don’t need intense workouts; moderate, consistent activity is most beneficial.
Optimal exercise for gut and mental health:
- Aerobic exercise: 30 minutes of brisk walking, cycling, or swimming 5 days weekly
- Strength training: 2-3 sessions weekly to reduce inflammation and improve insulin sensitivity
- Yoga: Especially beneficial for gut-brain axis through vagus nerve stimulation and stress reduction
- Tai chi or qigong: Combines movement with breathwork for optimal gut-brain benefits
The key is consistency over intensity. Even 10-minute movement breaks throughout the day accumulate significant benefits.
Stress Management: Protecting Your Gut-Brain Connection
Chronic stress is one of the most damaging factors for both gut health and mental wellness. When you’re stressed, blood flow diverts away from your digestive system, beneficial bacteria decline, and gut permeability increases.
Evidence-based stress reduction techniques:
- Deep breathing exercises: 5-10 minutes of diaphragmatic breathing 2-3 times daily
- Meditation or mindfulness: Start with 10 minutes daily using apps like Calm or Headspace
- Progressive muscle relaxation: Systematically tense and release muscle groups
- Nature exposure: Even 20 minutes in green spaces significantly reduces cortisol
- Gratitude practice: Writing three things you’re grateful for daily improves mood and gut function
- Cold exposure: Brief cold showers activate the vagus nerve and reduce inflammation
- Creative activities: Art, music, gardening, or crafting lower stress hormones
Your 30-Day Gut-Mood Transformation Plan
Ready to experience the gut-brain connection for yourself? Follow this progressive 30-day protocol:
First Week: Foundation Building
- Eliminate or significantly reduce processed foods, added sugars, and alcohol
- Add one fermented food daily (start with yogurt or kefir if new to fermented foods)
- Drink 64-80 ounces of water daily
- Establish consistent meal times
- Take a 10-minute walk after dinner
Second Week : Diversification
- Add a second fermented food or probiotic supplement
- Increase fiber intake to 25-30 grams daily with prebiotic foods
- Incorporate omega-3-rich fish 2-3 times this week
- Start a 5-minute morning breathing practice
- Aim for 7-8 hours of sleep nightly
Third Week : Optimization
- Add bone broth or L-glutamine supplement for gut lining repair
- Include polyphenol-rich foods at every meal (berries, green tea, dark chocolate)
- Establish a consistent eating window (e.g., 8 AM to 7 PM)
- Increase movement to 30 minutes daily
- Practice mindful eating (no screens, chew thoroughly)
Fourth Week : Integration and Fine-Tuning
- Continue all previous habits
- Add stress management practice (meditation, yoga, journaling)
- Experiment with meal timing that feels best for your energy and mood
- Assess what’s working and adjust accordingly
- Plan how to maintain these habits long-term
Timeline: When to Expect Mental Health Improvements
Understanding the timeline helps maintain realistic expectations and motivation:
Days 1-7: Better digestion, reduced bloating, slightly improved energy levels. Some people notice small mood improvements, especially if they’ve eliminated trigger foods.
Weeks 2-3: More stable energy throughout the day, improved sleep quality, reduced anxiety symptoms. Your gut bacteria are beginning to shift toward a healthier balance.
Weeks 4-8: Noticeable mood improvements, better stress resilience, clearer thinking, and improved focus. The changes in your microbiome composition become more substantial.
Months 3-6: Significant transformation in both gut diversity and mental wellness. Many people report feeling like their “old self” again or better than they have in years. Sustainable habit formation occurs.
Long-term (6+ months): Optimal gut-brain function with continued adherence. Your microbiome has adapted to your new lifestyle, supporting consistent mental clarity, emotional stability, and resilience.
Individual timelines vary based on starting point, consistency, stress levels, sleep quality, and other factors. Be patient and trust the process.
Gut Health Testing: Should You Consider It?
If you’ve implemented these strategies for 2-3 months without significant improvement, gut microbiome testing can provide valuable insights. These tests analyze your stool to identify bacterial composition, diversity, and potential imbalances.
When to consider testing:
- Persistent digestive issues alongside mental health symptoms
- History of antibiotic use or gut infections
- Autoimmune conditions
- Unexplained mood disorders not responding to treatment
- Desire for personalized gut health recommendations
Popular testing companies include Viome, Thorne, and Ombre. Discuss results with a functional medicine practitioner or registered dietitian who specializes in gut health for best interpretation and action plans.
Working with Healthcare Professionals
While improving gut health can significantly impact mental wellness, it’s not a replacement for professional mental health care. Consider working with:
- Psychiatrist or psychologist: For diagnosed mental health conditions
- Registered dietitian: Specializing in gut health or mental wellness
- Functional medicine doctor: For comprehensive gut-brain axis assessment
- Naturopathic doctor: For integrative approaches combining conventional and natural therapies
The most effective approach often combines professional mental health support with strategic gut health optimization.
Your Gut-Brain Connection Matters
Your mental health is too important to leave to chance. While therapy and medication have their rightful place in mental health treatment, supporting your gut-brain connection through food and lifestyle is a powerful, accessible strategy you can implement starting today.
This isn’t about perfection, restrictive dieting, or adding stress to your life. It’s about understanding that your body is an interconnected system where gut health profoundly influences how you think, feel, and experience life. By nourishing your microbiome with intention, you’re investing in your mental clarity, emotional stability, stress resilience, and overall quality of life.
The science is clear: the gut-brain axis represents one of the most exciting frontiers in mental health research and treatment. With every meal, every mindful breath, and every good night’s sleep, you’re either supporting or undermining this critical connection.
Your gut and brain are already in constant communication. Make sure they’re sharing good news.
Frequently Asked Questions About Gut Health and Mental Health
Q: How long does it take for gut health to improve mental health? Most people notice initial improvements within 2-4 weeks, with significant changes by 8-12 weeks of consistent gut-healthy habits.
Q: Can probiotics help with anxiety and depression? Research shows specific probiotic strains (psychobiotics) can reduce anxiety and depression symptoms, though results vary individually. They work best combined with dietary and lifestyle changes.
Q: What are the signs of an unhealthy gut? Common signs include bloating, gas, constipation, diarrhea, food intolerances, brain fog, mood swings, anxiety, fatigue, and skin issues like acne or eczema.
Q: Is the gut-brain connection scientifically proven? Yes. Extensive research confirms bidirectional communication between the gut and brain through neural, hormonal, and immune pathways. Major institutions including Harvard, Stanford, and Johns Hopkins study this connection.
Q: Should I take probiotics or eat fermented foods? Both are beneficial. Start with fermented foods for natural probiotic diversity, then consider supplements for targeted strains or if you don’t tolerate fermented foods well.
Q: Can antibiotics cause mental health problems? Antibiotics can disrupt gut bacteria balance, potentially contributing to mood changes. If you need antibiotics, take a high-quality probiotic during and after treatment (separated by 2-3 hours).
Q: What’s the best diet for gut and mental health? A whole-foods diet rich in fiber, fermented foods, omega-3s, and polyphenols while limiting processed foods, sugar, and alcohol. The Mediterranean diet is particularly well-researched for both gut and mental health.
#GutHealth #MentalHealth #GutBrainConnection #MentalWellness #HealthyGut #HealthyLifestyle #WellnessTips #SelfCare #HolisticHealth #FunctionalMedicine #CleanEating #HealthyLiving #MindfulEating #WellnessWednesday #HealthTips


